When is EMR performed?
- If a nodule (swelling) is seen in the inner lining (mucosa) of the oesophagus during endoscopy, the best thing is to remove it. There are two reasons for doing this:
- Diagnosis: The doctor cannot always tell what abnormality is present in a nodule. Removing it allows the pathologist to examine it under the microscope.
Treatment: nodules can have early cancer in them, so they are best removed if it is possible to do so
How is EMR done?
Various techniques are used for endoscopic mucosal resection. But they all do the same thing. They all remove the nodule.
The steps for EMR may include:
- Marking the area. This is particularly useful if the abnormality (nodule) is very small. It makes it easier to ensure that it is completely removed
- Injecting salt water or adrenaline under the nodule. This can make the treatment safer, particularly in areas that are more likely to bleed such as at the junction between the oesophagus and stomach. Adrenaline in particular can reduce the risk of bleeding
- Snaring the nodule. This is most often done by placing a specially designed loop or snare around the nodule. The snare is slowly closed whilst diathermy is given. This coagulates and stops and blood vessels bleeding. At the same time, it removes the abnormalityIf the nodule is big, it may be necessary to do more than one endoscopic mucosal resection to completely remove it. This is called piecemeal resection
Photographs of an oesophageal nodule and an EMR resection can be found on our picture gallery page. Please note that some people may find photographs of internal organs distressing. We have therefore not shown the photos on this page.
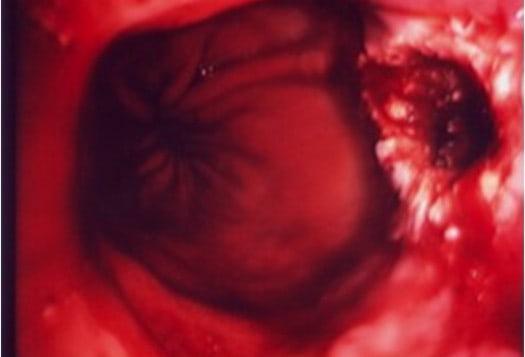
There is a visible nodule in this segment of Barrett’s oesophagus which will be removed by EMR

After removal of the nodule at EMR, there is a defect in the inner wall of the oesophagus. This heals spontaneously within 6 weeks. The patient usually suffers only minor discomfort for a few days after treatment
EMR findings
The specimen which is retrieved is sent to the pathologist for examination. In most cases, it will confirm dysplasia which is pre-cancerous. Further treatment can then be undertaken with endoscopy.
In a small number of people the endoscopic mucosal resection procedure will reveal that cancer is already present. If this happens, endoscopic treatment may no longer be the correct way forward, particularly if the cancer is already involving the submucosa (hyperlink to the word submucosa at top of this page).
If there is submucosal involvement, the doctor may recommend more extensive treatment to prevent the cancer spreading.
Risks of EMR
This procedure is safe.
In a small number of people, approximately one in ten, endoscopic mucosal resection can be complicated by minor bleeding. This is stopped by the doctor during the endoscopy itself.
If we were looking after you and you had a minor bleed, we would keep you in hospital for observation overnight.
In less than one in a hundred people, there can be major bleeding. This is treated by blood transfusion but it almost always stops by itself with no direct intervention. Rarely, the doctor will have to do another endoscopy or arrange for some other type of intervention to stop the bleeding.
Making a hole through the oesophageal wall (perforation) is very rare indeed. It happens in about one in 500 procedures.
If the nodule is very large, multiple EMRs can be done at the same endoscopy. This increases the risk of bleeding slightly. It also increases the risk of causing a stricture or narrowing of the oesophagus. This stricture may not become apparent for some weeks after the EMR.
How you will feel after EMR
EMR treatment is done as a day case endoscopy procedure. The patient goes home within 4 hours. Most people feel a little sore in the chest or back for between 3 and 7 days. Very occasionally, there is more extensive chest discomfort, particularly on swallowing, but this is unusual.
If a stricture develops, the patient may become aware that food gets stuck on swallowing. This may need further treatment to cure the problem.
We take great care to lessen the risk of getting a stricture. There are a few ways we can do this. If you need an EMR, please speak to us about the risks and how we manage them.
Follow Up after EMR
EMR is successful in removing all the dysplasia (pre-cancerous changes) in about one half of all patients treated. Even so, the Barrett’s oesophagus usually remains.
If there is residual Barrett’s, it needs to be removed entirely as one in three people will develop further dysplasia within five years.
We normally recommend patients have further treatment with HALO radiofrequency ablation following a successful EMR procedure.
For more information on Barrett’s oesophagus, please use the menu below to navigate through our pages
Please remember that endoscopic mucosal resection in the oesophagus should be done by experts. We offer this service. If you would like an appointment, please tell our office staff that you want to see a Barrett’s oesophagus expert. We will make sure you see the right person.
Why choose the London Gastroentrology Centre?
Same Week Appointments
Fast diagnosis and treatment leads to better outcomes for patients.
Confidentiality Assured
We take your privacy seriously. Your personal information is securely protected.
Choice of Payment Options
We are recognised by all major UK insurers. We also see self-funding patients. Please speak to our office staff for details.

 The oesophageal wall has three major layers, the inner lining (mucosa), the scaffold layer (sub-mucosa) and the outer muscular coat (muscularispropria)
The oesophageal wall has three major layers, the inner lining (mucosa), the scaffold layer (sub-mucosa) and the outer muscular coat (muscularispropria)